Michigan gets med-school boom, doctor bust
More doctors will be graduating from Michigan medical schools in the next decade. Whether that means more doctors practicing in Michigan is another matter.
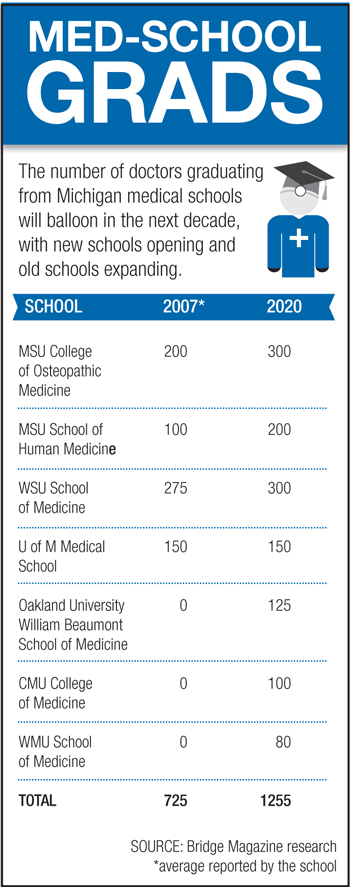
New medical schools have opened, or will open soon, at Oakland University, Central Michigan University and Western Michigan University. Michigan State University’s two medical schools also are greatly expanding their enrollment.
But more medical school grads may not alleviate Michigan’s chronic shortage of rural physicians, because the number of residencies -- the post-college, in-hospital training required to practice medicine -- remain capped by the federal government. Few are optimistic that the number of residencies will increase anytime soon. That probably means more Michigan medical students will leave the state for residency programs.
And most of them will never come back.
“But 2015, we will have more (medical school) graduates than we have residency positions,” predicts Peter Coggan, president of the Grand Rapids Medical Education and Resource Center. “It’s going to be a problem.”
Report: Doctor shortage looms
Michigan needs more doctors, a view repeated by administrators of the state’s established and new medical schools. The Center for Health Workforce Studies projects a shortage in Michigan of 4,400 doctors by 2020. More than a quarter of physicians currently practicing in the state are over age 60, meaning there will be huge pressure just to replace retirees, let alone increase the number of doctors.
 “There’s a critical shortage of physicians that’s going to get much worse,” said Dr. Hal Jenson, dean of the fledgling Western Michigan University School of Medicine. Without an increase in home-grown doctors, “we will be competing with the rest of the country to recruit physicians to Michigan.”
“There’s a critical shortage of physicians that’s going to get much worse,” said Dr. Hal Jenson, dean of the fledgling Western Michigan University School of Medicine. Without an increase in home-grown doctors, “we will be competing with the rest of the country to recruit physicians to Michigan.”
The state is facing a shortage of doctors in every discipline, says Dr. Robert Folberg, dean of the Oakland medical school. About 70 percent of the school's inaugural class is from Michigan, which Folberg hopes increases the odds of the physicians practicing in the state.
Central Michigan hopes to recruit students locally, too, with the goal of churning out about 100 doctors a year on campuses in Mt. Pleasant and Saginaw. “We have in Michigan developed a significant shortage of physicians,” says CMU College of Medicine Dean Ernie Yoder, “and that shortage contributes to problems accessing health care in rural areas.”
When Oakland University William Beaumont School of Medicine welcomed its first 50 students in the fall of 2011, it became the first medical school to open in the state in 47 years. CMU will open in 2013 and WMU will follow in 2014. Those three Michigan schools are among 18 opening around the country, part of the biggest U.S. medical school boom in decades.
By 2020, Michigan will be graduating about 1,250 medical school students a year – an increase of 73 percent in a decade.
There’s only one problem: Doctors can’t practice in Michigan without a residency, which typically lasts two years. And the number of those residencies in Michigan isn’t going up.
That’s critical, because more than 60 percent of physicians end up working within 100 miles of the site of their residency. For example, a CMU medical school grad with a residency in Florida is more likely to set up practice in Miami than Mt. Pleasant.
So, by increasing the number of medical school grads, but not simultaneously increasing the number of residencies, “you’re simply decreasing the likelihood that a kid who trains here will practice here,” said Oakland’s Folberg. “You’re training doctors to export them.”
Medical schools have no control over residencies, which are based at medical centers and take place after the students graduate. Residencies are primarily paid for through a combination of federal and state dollars. The federal government has had a cap on residencies since 1996.
Some hospitals do self-fund additional residency spots, because the young doctors serve an important role in health care -- and in their budgets.
“Not only do they see patients and often improve patient care, they ask questions, work on quality improvement projects, and they’re there at night,” said Dr. Aron Sousa, senior associate dean of the MSU College of Human Medicine. “It’s an attractive thing (for hospitals).”
Laura Appel of the Michigan Health & Hospital Association noted that residents are paid in the $40,000s or $50,000s and thereby provide "incredible value." And since residencies typically are located at hospitals serving disadvantaged populations, these doctors are a "staple" in care for patients under Medicaid and the uninsured.
But hospital budgets are tight, and most are unlikely to increase self-funded residency slots.
The increase in the number of in-state medical school grads could alter the composition of the residency corps, however, by pushing some international medical grads out of Michigan residency slots (about 200 international medical students nabbed Michigan residencies this year). But that still won’t affect the total spots available in the state.
Sousa puts it bluntly: The increase in medical school grads “won’t add to the number of physicians (practicing) in Michigan.
“There are a few residencies that aren’t filled now, but not many,” Sousa said. “It’s not a question of will there be more physicians -- it’s a question of whether your graduates will be able to find a residency.”
At present, virtually all medical school graduates in the United States find a residency through a national matching program. Some don’t get a residency in their preferred specialty, and a few fall through the cracks and wait a year.
That may change within a decade, as the number of medical school graduates is expected to surpass residencies nationally around 2015, said Coggan. “I fear we’ll encourage all these kids to go to med school and many will find residency programs out of state and we will lose their intellectual to the state, and that some will not be able to pick up a residency at all.
“I’m really concerned about the medical students who incur large education debts (often more than $200,000) and graduate without being able to practice medicine.”
Michigan could choose to increase spending on graduate medical education -- the state money used to fund residency programs. Instead, Gov. Rick Snyder proposed a cut that, with the loss of federal matching funds, would have amounted to $17 million less for the state’s 48 teaching hospitals.
“We have over 200 residents in training in our system – these residents are the safety net for our most vulnerable patients in Michigan,” Dr. Mark Hannis, director of medical education for Oakwood Healthcare System in Wayne County, testified in Lansing recently.
Hannis told the House Appropriations Subcommittee on Department of Community Health Appropriations that state and federal funding for residency training has been flat for the past decade, despite rising costs and increasing requirements placed on teaching programs. “Teaching hospitals like Oakwood have (already) been doing more with less,” Hannis said.
Instead of a $17 million cut, legislators agreed to an $8 million increase. And for every $1 the state invests in graduate medical education, it gets $1.97 in federal funds, MHA's Appel explained.
Figures provided by the MHA show a trend of declining support over the long term. In 1995, GME total funding was $222 million, and levels fell off from there to the $168 million level during much of the 2000s. For 2013, the total will be $163 million -- or about 50 percent of the 1995 level, when adjusted for inflation.
Medical schools are considered good business for communities, with the total economic impact in Michigan estimated at $24.2 billion in 2008, according to a study by the Association of American Medical Colleges.
Michigan’s new medical schools won’t have a dramatic immediate economic impact, because new hospitals aren’t being built with them. Likewise, the state isn’t likely to be on the hook for more money because of more medical schools popping up at public universities. Western Michigan's and Oakland's are private medical schools within public universities, meaning state money isn’t funding the endeavors. Start-up costs for CMU’s medical school came in large part from donations, and administrators expect the school to be self-supporting by the time the first or second classes graduate.
“People need to understand that physicians need to come from somewhere,” says MSU’s Sousa. “We want them to be well trained, and that’s what residencies do. There’s a huge amount of learning that takes place in residencies.
“If you want somebody to take care of you 20 years from now,” Sousa says, “they need to be trained now.”
Senior Writer Ron French joined Bridge in 2011 after having won more than 40 national and state journalism awards since he joined the Detroit News in 1995. French has a long track record of uncovering emerging issues and changing the public policy debate through his work. In 2006, he foretold the coming crisis in the auto industry in a special report detailing how worker health-care costs threatened to bankrupt General Motors.
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!

