Man v. Microbe: Drug-resistant superbugs gain a toehold in Michigan
DETROIT—The whimsical stuffed toys next to his lab belie the dangers that Dr. Robert Tibbetts studies.
The critters are kid-friendly replicas of deadly microbes, including so-called superbugs — nightmare pathogens that kill, in part, because of their ability to evade antibiotics and other drugs designed to halt their spread.

Quietly, slowly — “we are running out of options,” Tibbetts said of the threat, echoing the alarm raised in November by the World Health Organization, which criticized doctors’ (and veterinarians’) overreliance on antibiotics in fueling the growth of drug-resistant pathogens.
Related:
- Detroit hospital stops admitting patients to control rare fungus outbreak
- Michigan baby formula factory focus of FDA probe after infant illnesses
In Michigan, that alarm is more than theoretical.
Consider:
- Last month, a Detroit hospital stopped taking patients temporarily as it tried to contain an outbreak of a rare, but potentially deadly fungus, Candida auris. Normally confined to long-term care facilities, C. auris cases have been reported most recently in COVID units at acute care hospitals, according to the U.S. Centers for Disease Control and Prevention.
- Studies show that potentially-lethal Cronobacter sakazakii — the bacteria associated with possibly tainted baby formula from a Michigan facility this year — also is growing more resistant to antibiotic drugs.
- Another threat is vancomycin-Resistant Staphylococcus aureus (VRSA). The first U.S. case was detected 20 years ago in a 40-year-old Michigan man with diabetes — apparently introduced via a dialysis catheter. The Michigan case was the first clue that VRSA, discovered eight years earlier in Japan, had arrived in the United States.
- Of the 16 total U.S. cases of VRSA reported through last year, nine involved Michigan patients who developed infections after surgeries in cases such as a “toe wound,” according to a January special report by the U.S. Centers for Disease Control and Prevention.
More than 2.8 million antibiotic-resistant infections occur in the U.S. each year, leading to 35,000 deaths, according to a 2019 Antibiotic Resistance (AR) Threats Report by the CDC.
Historically considered a risk primarily to seniors and people with chronic conditions, drug-resistant microbes have become a growing threat to healthier residents, too, said Tibbetts, an associate director of microbiology at Henry Ford Hospital in Detroit who helps track pathogens.

“It’s unfortunate, because you could cut yourself swimming one day and the next thing you know…you’ve got things like necrotizing fasciitis (flesh-eating disease). You’re losing your limbs because they have to amputate because we can't treat some of these infections,” he said.
VRSA is one of many concerns, said Dr. Natasha Bagdasarian, Michigan’s chief medical executive.
It’s “the next step, in terms of resistance” among the common S. aureus, which also includes methicillin-resistant Staphylococcus aureus, or MRSA, which caused an estimated 70,557 infections and 4,337 deaths in Michigan between 2002 and 2008, according to one review of Michigan hospital data.
To be sure, these superbugs remain most dangerous to the chronically ill and older patients, but it’s their ability to constantly evolve to dodge drugs that worries Bagdasarian, Tibbetts and others.
“These organisms have a way of becoming more prevalent and extending their reach,” Bagdasarian said.
Arms race
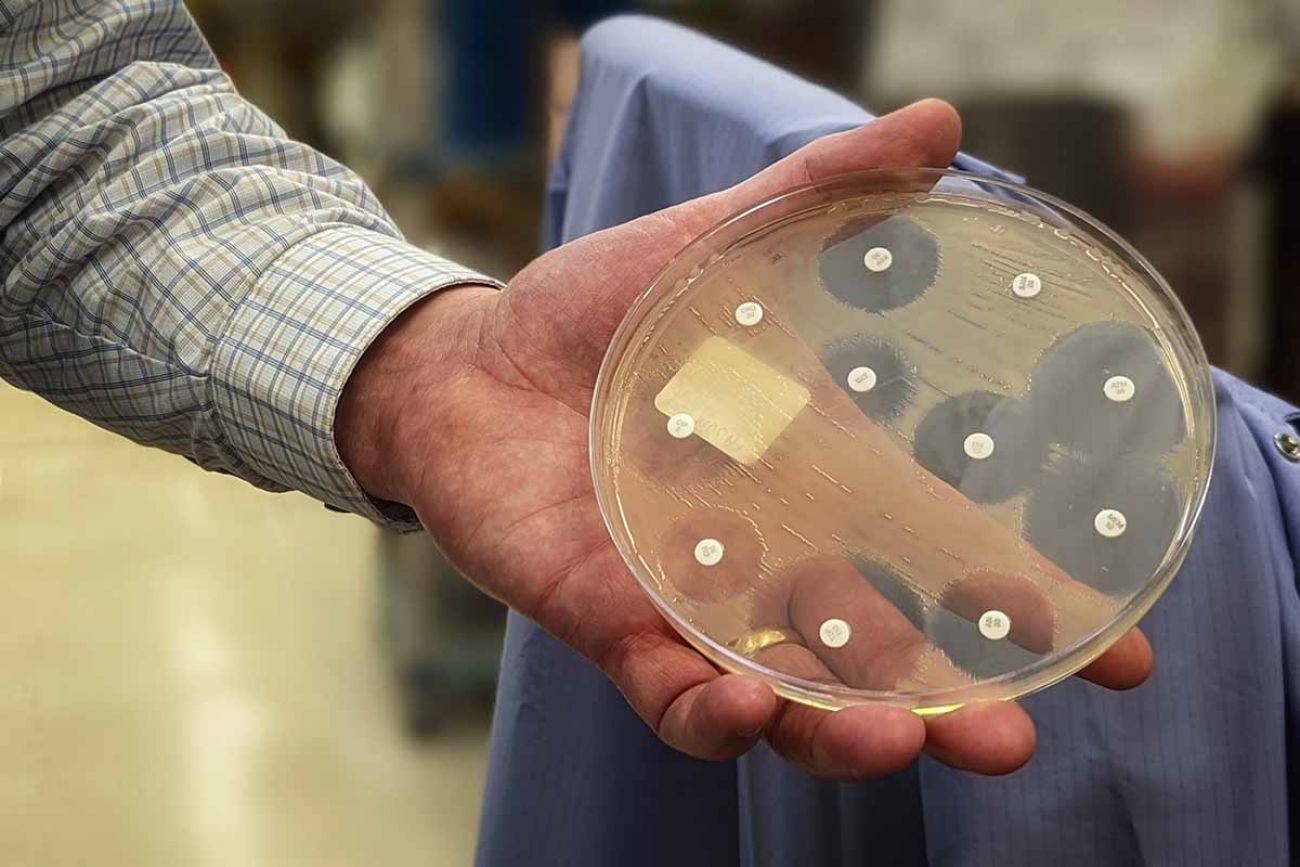
Over the decades, the power of antibiotics has become their weakness — the result of an microscopic arms race that began with Dr. Alexander Fleming’s discovery of penicillin in a moldy petri dish more than 90 years ago.
Before that 1928 scientific accident, which led to the development of antibiotics, even healthy people “routinely” died from common infections, such as strep throat or urinary tract infections.
But Fleming’s penicillin and other medicines have been so effective that many medical professionals routinely overprescribe them, and many patients demand them, even for such conditions as the common cold (though they are ineffective against cold viruses). So too, the agribusiness industry uses them by the ton to prevent disease in livestock.
At least two studies found that 30 percent of all antibiotics prescribed in U.S. acute-care hospitals are either unnecessary or less than ideal.
And researchers reviewing medical records of 11,784 children in U.S. hospitals found that 1-in-4 who received antibiotics did not need them or had them incorrectly prescribed, according to a study published in 2020 in the Clinical Infectious Diseases, a journal of the Infectious Diseases Society of America.
Over time, microbes adapted and evolved in response to these and other antimicrobial medications, growing resistant to the drugs designed to kill them.
Antibiotics, in particular, are too often prescribed as a preventative measure, when the patient’s own body would likely fight off any infection — in dental offices after a tooth extraction, for example.
Dentists “don't see the downstream effects, which is drug-resistant bacteria and other harm to patients,” said Dr. Allison Weinmann, medical director of Henry Ford Health’s Antimicrobial Stewardship Program. The program focuses on providing more narrowly prescribing antibiotics — “the right antibiotic at the right time with the right dose and for the right duration,” she said.
Hospitals across the state and nation have implemented Antibiotic Stewardship programs to deal with the growing threat of drug-resistant pathogens.
The overuse of antibiotics also can endanger the individual patients.
Antibiotics kill indiscriminately. A doctor’s target may be a specific microbe behind an infection, and the drug, indeed, may stop the infection. But in doing so, it also could also throw off a person’s unique microbiome — the countless trillions of microbes that, for the most part, coexist peacefully and keep pathogens, or disease-causing microbes, in check.
“Especially with broad-spectrum antibiotics, you're wiping out not just the organism of concern, but a good chunk of your microbiome a lot of times,” said the state’s Bagdasarian. “Once you disrupt this microbiome — these organisms living in balance — then you can have proliferation of pathogens.”
With each new generation of pathogens comes the potential for genetic mutations that outmaneuver antibiotics, reducing the arsenal to fight them, said Dr. Varsha Moudgal, associate chief medical officer for Trinity Health St. Joseph Mercy Livingston.
“Bacteria and fungi will adapt to overcome the pressure from the antibiotics or antifungals designed to kill them,” she said.
With too many antibiotics, a person’s own body can grow vulnerable to other deadly infectious threats.
Consider the toxin-producing Clostridioides difficile, a germ that causes diarrhea and colitis.
It’s not typically considered drug-resistant, but when a person has used antibiotics so often they have lost their potency, C. diff can take hold in the gut. C. diff is the leading cause of infectious diarrhea in healthcare settings, and was linked to 1,296 deaths in Michigan between 2015 and 2019, according to a state review of cases.
The experts interviewed by Bridge all agreed that doctors need to be more precise in the medications they prescribe.
But patients also have a role to play, they said.
Patients should inform doctors, dentists and others they’re fine with using antibiotics only when necessary. It’s also important to take a full prescription as prescribed. Ending a course of treatment early means the infection may return stronger than before.

Antibiotics have been so ubiquitous for years that doctors often prescribe them without knowing what organism they’re targeting. And, Moudgal said, “It’s not unusual for a patient to go into a doctor’s office and demand antibiotics.”
Every time that happens, the doctor — sometimes with a full waiting room — has a choice: A lengthy conversation to explain antibiotic resistance and all the ways prescribing an antibiotic will likely will do more harm than good, or — as Henry Ford’s Weinmann notes, they can have a “much shorter conversation to say ‘Here's an antibiotic.’
“You would have a better time and faster time finding Jimmy Hoffa than explaining to a mother of a sick child or a patient who has a UTI (urinary tract infection) that you're not going to treat them” with the antibiotic they expect, said Tibbetts.
What’s on your plate
Antibiotics also enter our systems through the foods we eat.
They are used to prevent infection and promote growth in animals. Consequently, “livestock have become a reservoir of antimicrobial-resistant bacterial strains and genes,” according to Animal Frontiers, a publication for animal scientists. The antibiotic-resistant bacteria transfers to humans in meat or when animal waste containing drug-resistant bacteria seeps into the surrounding environment.
“And pigs are raised on antibiotics, not because they’ve got infections, but because it makes them grow quicker and fatter,” said Henry Ford’s Weinmann. “Then we’re eating meat that has drug-resistant bacteria, and it becomes part of our flora,” she said.
Using data from 41 countries, a 2020 study estimated more than 93 tons of antimicrobials were used in chicken, cattle and pigs in 2017, a number expected to grow to 104 tons by 2030.
“We’re all linked globally,” said Trinity’s Moudgal. If drug-resistant microorganisms continue to gain traction, he said, “it truly can be catastrophic.”
The U.S. Centers for Disease Control and Prevention lists nearly two dozen specific antibiotic resistance threats. Several Michigan experts listed some of their top concerns. Among them:
Multidrug resistant Candida auris
A rare fungus discovered in Japan in 2009, Candida auris is listed as one of five “urgent threats” among drug-resistant microorganisms, according to the CDC.
C. auris was recently detected at a Detroit hospital. Select Specialty Hospital – Northwest Detroit stopped accepting new patients in April to curb the spread. C. auris poses no threat to the general public, but can be deadly among vulnerable patients.
None of the Detroit cases were fatal, but it has been estimated that 30–60 percent of people with C. auris infections die, according to the CDC.
VRSA
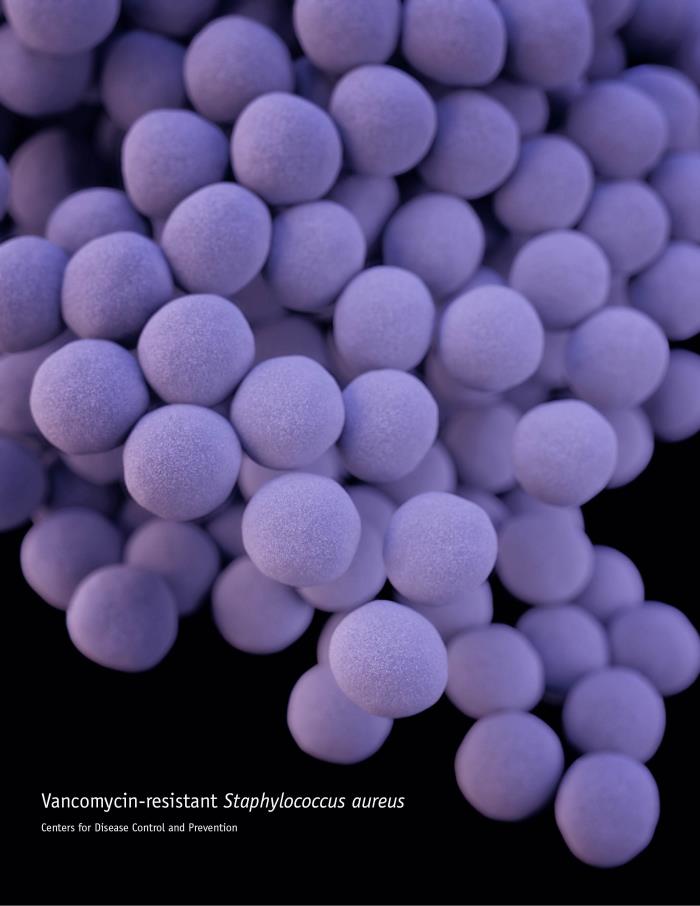
Michigan reported the first reported U.S. case of vancomycin-Resistant Staphylococcus aureus (VRSA) in 2002. It was detected in a 40-year-old Michigan man with diabetes, the result of his dialysis catheter. Of the 16 total cases reported though last year, nine were in Michigan.
Methicillin resistant S. aureus, or MRSA
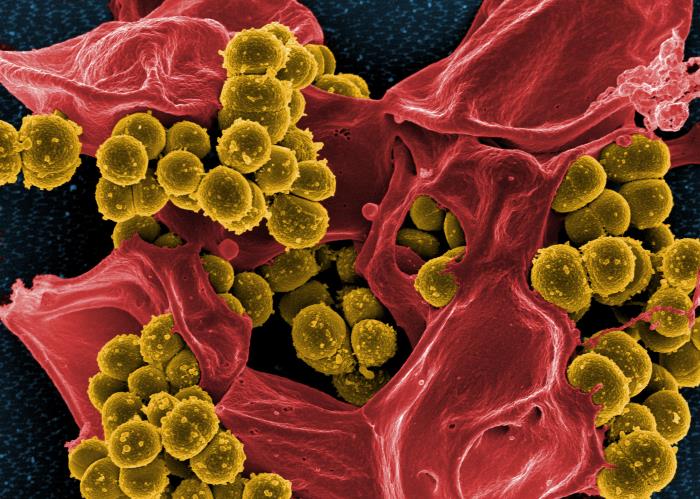
Staphylococcus aureus is one of the most common pathogens in health-care facilities, but it also can enter the body outside health facilities — through a cut, burn or scrape, for example. Infections may begin as a small bump that’s tender, swollen, or even warm to the touch, but also can be deadly.
Nationally, an estimated 119,247 S. aureus bloodstream infections were confirmed in 2017, including 19,832 associated deaths, according to the CDC. In Michigan, 70,557 patients had MRSA infections between 2002 and 2008, according to one review.
Vancomycin resistant Enterococcus, or VRE
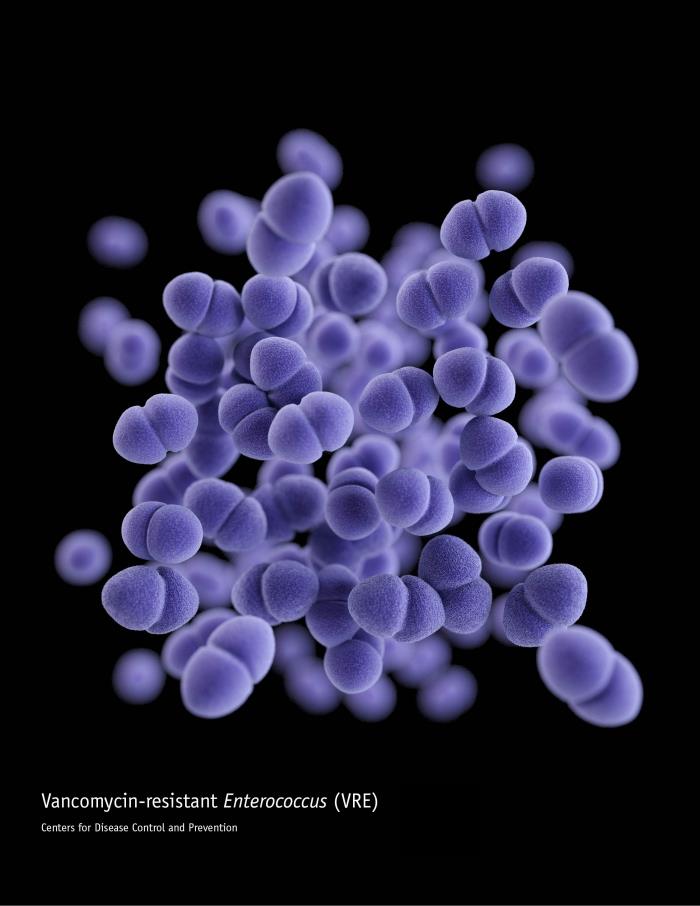
Enterococci bacteria are normal in the human intestines, female genital tract, as well as in soil and water, and a person’s microbiome usually keeps it in check. But among people with chronic conditions, weakened immune systems and open wounds, they can trigger infection.
In 2015, one Michigan study noted concerns about a large “community reservoir” of VRE in southeast Michigan, confirming concerns that people living outside the home (in nursing homes, for example), with open wounds, and with prior use of antibiotics are most vulnerable. Two years later, VRE caused an estimated 54,500 infections in U.S. hospitals and was associated with about 5,400 deaths, according to the 2019 CDC Antiobiotics Resistance Threats in the U.S. report.
Carbapenem-resistant Enterobacterales

Enterobacterales bacteria such as E. coli can drive infections in health care settings. Doctors often prescribe a class of antibiotics known as Carbapenems to treat them. But in 2017, the CDC recorded more than 13,000 U.S. cases of Carbapenem-resistant Enterobacterales (CRE’s) in hospitalized patients and roughly 1,100 deaths.
Another Carbapenem-resistant bacteria, Pseudomonas aeruginosa, arrived in 18 states, including Michigan, in 2018 and 2019 via medical tourists who underwent bariatric surgery in Tijuana, Mexico. Most of the 38 patients were operated on by one surgeon, according to an investigation published in the peer-reviewed publication, Emerging Infectious Diseases.
Clostridioides difficile

The Clostridioides difficile bacterium is not typically resistant but people who have had multiple antibiotics are most susceptible. Associated with deadly diarrhea and an inflammation of the colon, C. diff colitis is associated with 223,900 infections and 12,800 deaths nationally each year.
It’s most deadly among older people. About one in 11 people 65 and older who are diagnosed will die within a month of diagnosis.
In Michigan, C. diff. was associated with 1,296 deaths in Michigan between 2015 and 2019 — with death rates far higher for older people.
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!





